14
Dec
2020
What Is Hypotonia? – And 14 Other Questions You Need To Ask
What is hypotonia?
Parenting forces you to ask a countless number of questions you never expected to even consider. And that’s certainly one of them.
If the word hypotonia recently entered your vocabulary, you’re probably equal parts concerned and confused.
Let’s fix that.
In this post, we’ll take a deep dive into the world of hypotonia.
You can also find a shorter, simpler explanation to share with friends and family.
What Is The Definition Of Hypotonia?
Hypotonia is a decreased level of muscle tone. The severity of that decrease, as well as the body part(s) most impacted, varies from child to child.
That hypotonia definition is accurate, but it doesn’t tell the whole story. Far from it. You want to know about the real-life implications. Let’s dig deeper.
What Is Muscle Tone?
Muscle tone is the amount of tension in a muscle when it’s at rest. That last part is key because people often confusion muscle tone with muscle strength.
You can think of it this way. Strength is active. Tone is passive.
For people who prefer the hands-on approach, try this. Relax your arm and then pinch your bicep. It doesn’t matter how infrequently you visit the gym. Everyone has a certain level of tension in their muscles. That’s tone.
In the case of your child, that tension is decreased.
So Is My Child Is Just Weak?
Absolutely not.
Don’t let that misconception take root in your mind (or the minds of others.)
Can there be a connection between hypotonia and weakness? Sure, but that’s just cause and effect. Muscles may fail to develop proper strength if they’re not activated properly or used often enough. But that’s not what hypotonia is. It’s just a result.
What Causes Hypotonia?
The answer to this question probably isn’t as simple as you hoped. That’s because of two specific reasons:
- Hypotonia is linked to hundreds of different medical conditions
- Hypotonia is most often a symptom rather than the overarching diagnosis
If that second point is confusing, think in these terms. Something like Down syndrome is the common cold and hypotonia is the sniffles. One results in the other.
The causes of hypotonia can range from chromosomal abnormalities to a brain injury. Common diagnoses include:
- Down syndrome
- Cerebral palsy
- Prader-Willi syndrome
- Tay-Sachs disease
- Angelman syndrome
- Ehlers-Danlos syndrome
- Joubert syndrome
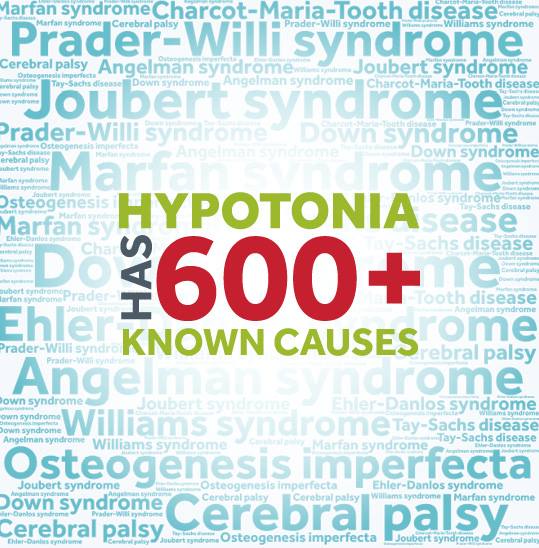
If it’s unclear why your little one has low tone, tests are available. Just know that getting a definitive answer isn’t guaranteed.
What Is Benign Congenital Hypotonia?
There are also instances of low muscle tone that seem to be without cause. It just is. This is called benign congenital hypotonia.
What Hypotonia Symptoms Can I Expect?
Hypotonia impacts everyone differently.
Even if you met another parent whose child has low tone, chances are your experiences would be quite different.
This is because:
- Hypotonia can range from mild to severe
- Hypotonia can impact different parts of the body
- Hypotonia can be just one of the symptoms associated with a diagnosis
But in general, common symptom categories include:
Delays
Kids often reach fine and gross motor skill milestones more slowly than peers
Instability
Muscle laxity and an increased range of motion can cause kids to feel less stable
Exhaustion
Hypotonia often requires extra effort just to keep up
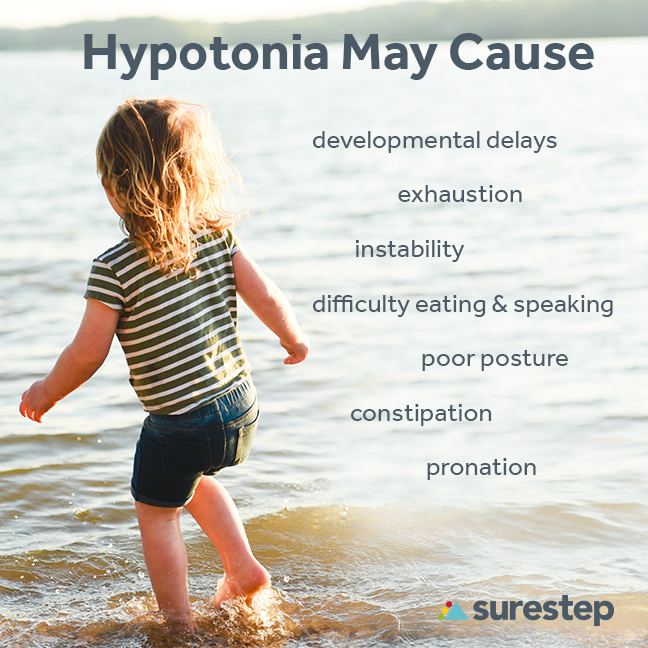
What About Pronation?
As kids get a little older, one of the most common signs of hypotonia that parents notice is pronation. This is an inward roll of the ankle that forces a child to stand and walk on the inside of his or her feet.
And while it may look like a minor obstacle, it actually throws off your child’s alignment and causes a chain reaction up the body.
Here’s an easy, visual way to check. Have your child stand barefoot and then look from directly behind them. If you see pinky toes but no big toes, your child pronates.

What Are Other Common Questions?
Your head is probably swimming with questions. Here are a few more you may be asking.
Can A Child Outgrow Hypotonia? Is There A Cure?
What do time, medication, surgery, weight training, and superfoods all have in common?
They won’t drastically improve your child’s muscle tone.
Muscle strength can be gained and lost, but tone doesn’t really change.
Your child will carry hypotonia into adulthood. That seems to be contradicted with any huge milestone breakthrough.
But instead, what you’re seeing is resilience. Kids are extremely adaptable. They learn how to work within their own limitations.
Just remember, even if you’re seeing gradual improvements, your child may still need help.
Will My Child Ever Walk?
It’s impossible to answer that question with 100% accuracy.
Hypotonia ranges in severity. Each child is unique. And there are other factors to consider with any diagnosis.
But in general, many, many kids do take those first steps.
There just may be delays, therapy, orthotics, and extra effort along the way.

Will My Child Have A Normal Life?
If you polled a hundred people, you’ll get a hundred different answers of what “normal” is.
Will there be obstacles, detours, and a few tears along the way? Probably.
But none of that means your child can’t have a fulfilling, productive, and beautiful life.
After all, hypotonia will teach your little one to be a fighter. And that’s a skill that plenty of people never develop.
What Should I Do Now?
Wait and see.
That’s the most common advice handed out by friends, family, and medical professionals.
But doing nothing changes nothing.
And for parents who follow this advice, the gap between their kid and peers tends to grow.
So if your parental intuition whispers that something is wrong, you don’t have to settle for one professional opinion.
Getting a second or third never hurt.
How Can I Help? What Are The Treatment Options For Hypotonia?
That’s the big question. And while the answer can vary, the best options typically fall into two categories.
They work well individually but are often best when paired together.
Physical Therapy

An experienced pediatric physical therapist will guide your child through activities and experiences that often feel like play.
The growth is incremental. But given enough time and commitment, your little one will gain strength, coordination, and balance.
Surestep SMOs
Surestep SMOs are braces specifically designed to treat pronation caused by hypotonia.
They gently compress your child’s foot and ankle, which helps:
- Increase stability
- Improve alignment
- Build confidence
And because they’re custom-made, you’ll first need to get a referral from your doctor.

So, what is hypotonia?
It’s a layered, complex question.
But armed with information, professional help, and a supportive family, your child can be setup for success.
Does my child need SMOs? Ask yourself these 7 questions.